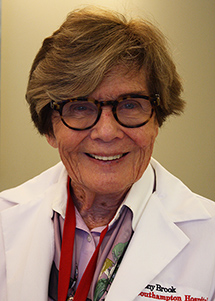
 Janet O'Grady, MSRD, CDE, CDN, is a multifaceted registered dietitian with more than 35 years of clinical nutrition experience. Since 2012, she has served as the sole diabetes coordinator and educator at Stony Brook Southampton Hospital, where she develops individualized treatment plans for patients to help them manage the disease. Additionally, she runs a monthly educational support program, “Living with Diabetes,” that is certified by the American Diabetes Association. She is also a dietitian on staff with Meeting House Lane Medical Practice.
Janet O'Grady, MSRD, CDE, CDN, is a multifaceted registered dietitian with more than 35 years of clinical nutrition experience. Since 2012, she has served as the sole diabetes coordinator and educator at Stony Brook Southampton Hospital, where she develops individualized treatment plans for patients to help them manage the disease. Additionally, she runs a monthly educational support program, “Living with Diabetes,” that is certified by the American Diabetes Association. She is also a dietitian on staff with Meeting House Lane Medical Practice.
Janet O'Grady sees patients in Southampton. To make an appointment, please call (631) 726-8357.
What does it mean to have diabetes?
Diabetes is a disorder where the body does not make or use insulin correctly. Insulin is a hormone your body uses to turn the food you eat into energy—when insulin is out of balance, your whole body is out of balance. This results in impaired metabolism of carbohydrates and protein, which leads to elevated levels of glucose in the blood and urine. It’s sometimes thought of as just having “a little bit of sugar in the blood,” but this is only one component of the disease.
What is the difference between Type I and Type II diabetes?
Type I diabetes is an autoimmune disease where the body’s immune system mistakenly attacks and destroys pancreatic beta cells. This results in the pancreas producing too little insulin and then, eventually, none at all. Type II diabetes is a metabolic disorder in which the body does not properly use insulin or produce insulin in the right amounts. The cells of people with Type II diabetes do not use insulin as supplied by the pancreas, so the ability for the organ to make insulin decreases over time.
What are the symptoms of diabetes?
Diabetes can sometimes be called a “silent disease,” as symptoms may not exhibit until blood sugars are grossly elevated. Symptoms include frequent urination, increased thirst and hunger, blurred vision, and poor wound healing caused by elevated blood glucose levels, or hyperglycemia. People also experience fatigue, which reflects the body’s inability to use insulin effectively. Without insulin, blood glucose cannot enter the cells to provide energy. Frequently, but not always, people with Type II diabetes may be overweight or obese, while people with Type I diabetes may experience weight loss.
What are the causes of diabetes, and how can it be managed?
The good news is that today diabetes can be managed and people can lead happy, healthy lives. Self-management is the key to staying on track, and our program at Stony Brook Southampton Hospital can help with that.
Heredity plays a role in causing Type I diabetes, but the exact cause is variable and may involve an individual’s race/ethnicity, geography, history of viral infections, and other autoimmune conditions. Type II tends to be present in overweight and obese people, certain ethnic groups, families with a history of Type II, and women with a history of gestational diabetes. Nine in 10 people with diabetes have Type II, and most people who are diagnosed are over the age of 40, although it is becoming more common in children.
Managing Type I diabetes revolves mainly around regular insulin injection, blood glucose monitoring, physical activity, and making healthy food choices. Managing Type II diabetes involves focusing on lifestyle behaviors, education and support, and medications if warranted. For the extreme obese patient with diabetes where dieting has failed, medications and surgical intervention might be recommended.
What are the health complications of diabetes?
Diabetes, when untreated, can lead to serious health problems. Hyperglycemia can damage large blood vessels and ultimately lead to stroke, heart attack, and loss of circulation in the arms and legs. Hyperglycemia can also damage small blood vessels and nerves, causing blindness and kidney disease. Open wounds or sores on the feet, known as diabetic foot ulcers, can form and may lead to hospitalization if infected, as they heal slowly.
Recent literature indicates that in individuals ages 40 or older, diabetes is linked to dementia and cognitive dysfunction. It’s also shown to increase the risk of osteoarthritis, osteopenia, and rheumatoid arthritis.
Again, the good news is that the tools available for diabetes care continue to improve and patients have choices when it comes to managing diabetes.

